Mouth Ulcers: Causes, Symptoms and Treatments
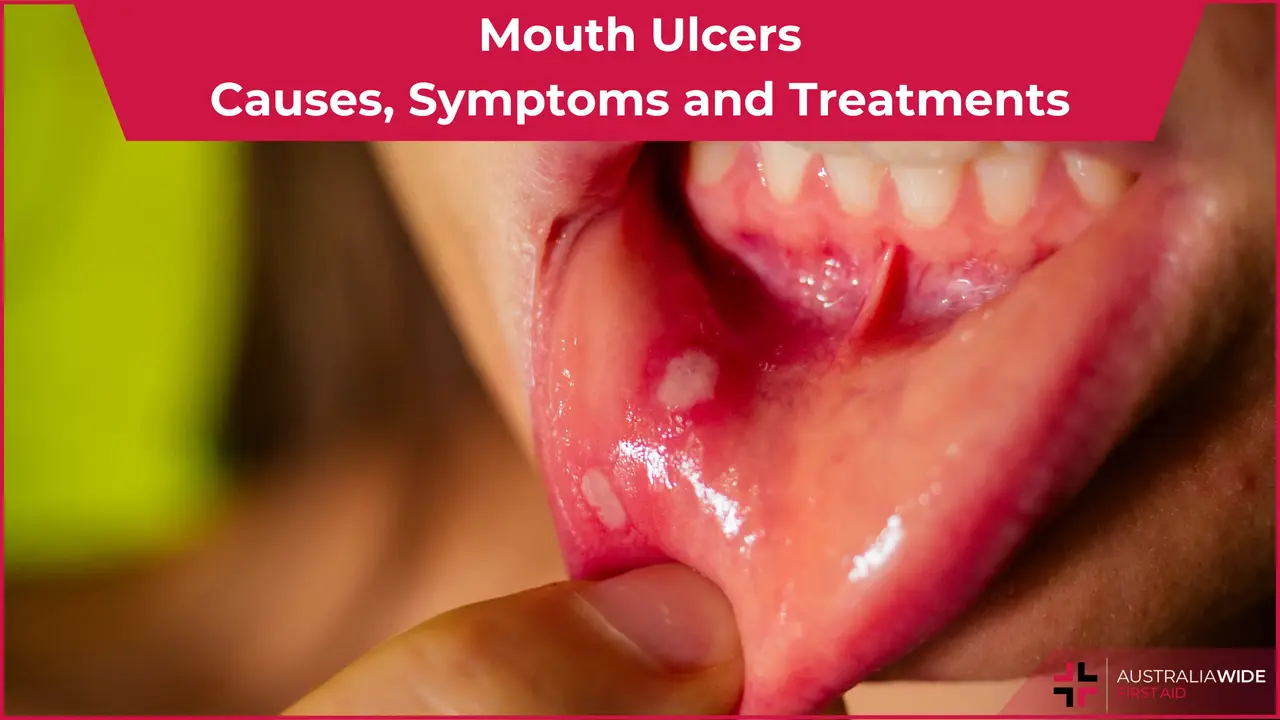
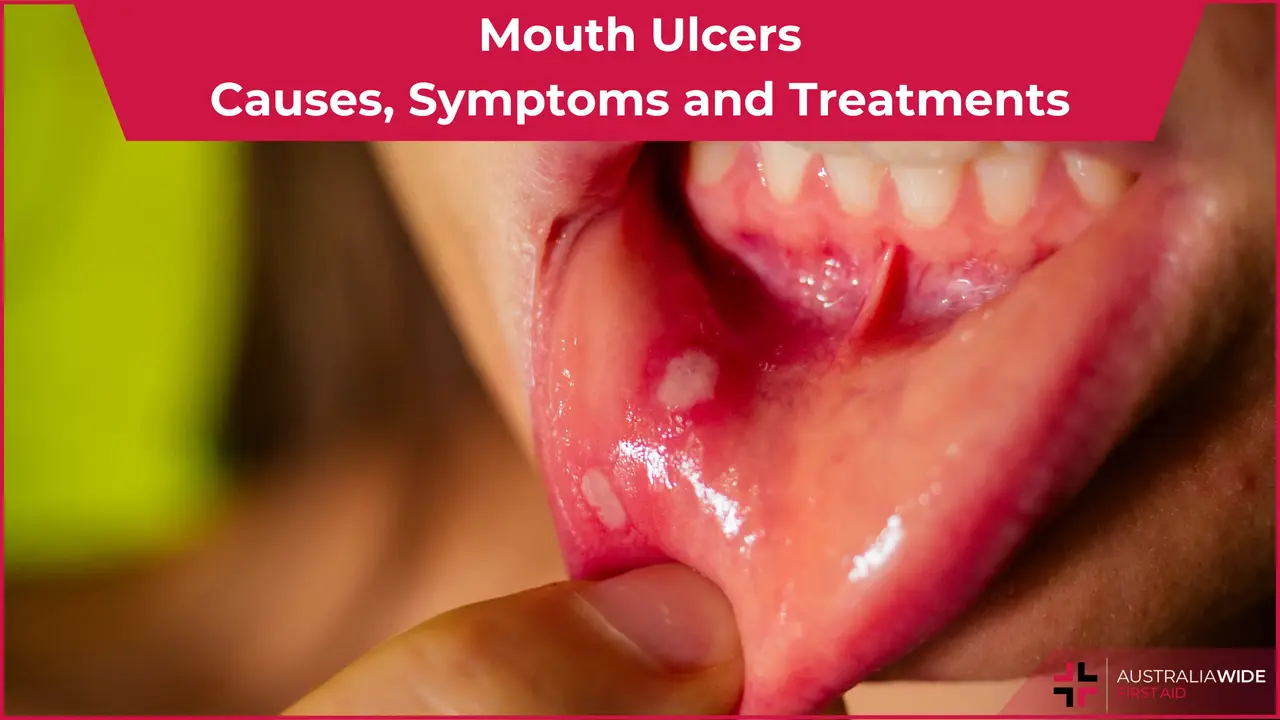
Mouth ulcers, also referred to as canker sores or aphthous ulcers, are small, painful lesions that commonly develop within the mouth, including the gums and tongue.
Typically displaying a white or yellow centre surrounded by inflamed red tissues, leading to persistent discomfort.
They can significantly disrupt daily activities like eating, drinking, and speaking.
While generally benign and non-contagious, these ulcers may sometimes persist for a week or two, causing prolonged pain and inconvenience.
In such cases, seeking prompt dental and medical care becomes paramount.
Mouth ulcers can be classified into several types based on their causes and characteristics:
Minor Aphthous Ulcers
These are the most common type of mouth ulcers, typically small (less than 1 cm) and shallow, appearing on the inside of the lips, cheeks, or under the tongue. Although painful, they usually heal within 1 to 2 weeks without scarring.
Major Aphthous Ulcers
Unlike minor ulcers, major aphthous ulcers are larger and deeper, often exceeding 1 cm in diameter. They can be extremely painful and may take several weeks to heal, with scarring being more likely.
Herpetiform Ulcers
Despite their name, herpetiform ulcers are not caused by the herpes virus. They are characterized by clusters of tiny ulcers that merge to form a larger sore. These ulcers are often very painful and tend to recur frequently.
Traumatic Ulcers
Resulting from physical injury or irritation to the mouth tissues, traumatic ulcers are usually shallow and heal relatively quickly once the source of trauma is removed. This can include accidental biting, sharp edges of dental appliances, or aggressive tooth brushing.
Drug-Induced Ulcers
Certain medications, such as NSAIDs, chemotherapy drugs, and some oral medications, can cause mouth ulcers as a side effect. These ulcers may resemble minor aphthous ulcers and typically resolve once the medication is discontinued.
Infectious Ulcers
Caused by viral infections like herpes simplex virus or bacterial infections like syphilis, infectious ulcers may be accompanied by other symptoms such as fever and swollen lymph nodes.
Systemic Disease-Related Ulcers
Some systemic conditions, including inflammatory bowel disease, Bechet's disease, and autoimmune disorders, can present with oral ulcers as one of their symptoms. Understanding the type of mouth ulcer a person is experiencing is crucial for determining the appropriate treatment and management. Seeking advice from a healthcare professional is essential for accurate diagnosis and individualised care.
Signs and symptoms of mouth ulcers vary depending on the type and cause of the ulcer.
However, the most common presentation of mouth ulcers is as follows:
Symptoms Of Herpetiform Ulcers:
All these factors can significantly contribute to the occurrence of mouth ulcers.
Identification of these risk factors and treatment of underlying causes remains the foundation of treating mouth ulcers.
Therefore, it is essential to consult a healthcare professional promptly for proper management.
By following these recommendations and seeking guidance you can effectively manage mouth ulcers and promote oral health.
Mouth ulcers are typically not a cause for immediate concern and can often be managed at home.
However, there are certain situations where it may be advisable to seek medical or dental attention.
See a Dentist if:
See a Doctor (General Practitioner or Primary Care Physician) if:
In severe cases where mouth ulcers become exceptionally large and painful, medical intervention may be necessary.
If your ulcer persists without improvement and the pain worsens, seek care to address any underlying issues.
In general, if you are unsure whether to see a doctor or a dentist for your mouth ulcers, it is advisable to start by consulting with your dentist. They can assess your oral health and refer you to a physician for further management, if necessary.

March 25, 2025
Explore non-traditional paths to sobriety, including mindfulness, yoga, nutritional therapy, and community-based support, for a personalized approach to recovery.
September 7, 2022
Menopause is the final period, when a woman, trans man, or non-binary person assigned female at birth's ovaries run out of eggs and the body can no longer ovulate. Menopause comes with several symptoms, complications, and treatment options.
July 26, 2024
Transcutaneous Electrical Nerve Stimulation (TENS) is a therapeutic method of pain relief. It utilises an electrical device that emits electrical currents and streams the impulses via electrode patches attached to the skin.